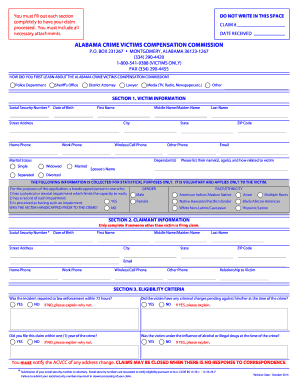
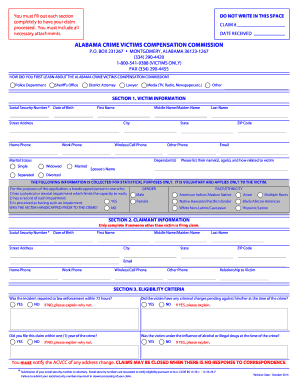
Enter your official contact and identification details. Apply a check mark to point the answer wherever necessary. Double check all the fillable fields to ensure full accuracy. Utilize the Sign Tool to add and create your electronic signature to signNow the Authorization for Use/Disclosure of Protected HEvalth Information.
Full Answer
What is an authorization for the disclosure of health information?
General Authorizations: In accordance with §164.508 of the privacy rule, an authorization for the disclosure of health information may be combined with another authorization. For example, a patient may request lab results be disclosed to two different family members (living in separate residences) on the same form.
What are the rules for protected health information?
The rules, which are part of the Health Insurance Portability & Accountability Act (HIPAA), restrict access to protected health information by anyone not involved in treatment, payment or health care operations without the patient's permission. Protected health information is information that is identifiable to an individual.
What is protected health information under HIPAA?
Protected health information is information that is identifiable to an individual. Some examples of individual identifiers are: In most instances, the Department must have the individual's authorization in order to disclose their health information. The HIPAA law lists specific requirements that an authorization form must meet.
What are the new rules for medical records privacy?
New rules that help to protect the privacy of your medical records took effect April 14, 2003. The rules, which are part of the Health Insurance Portability & Accountability Act (HIPAA), restrict access to protected health information by anyone not involved in treatment, payment or health care operations without the patient's permission.
How do you fill out authorization for release of protected health information?
A: You must write the form in plain language and include the following parts:A description of the information that you will use or disclose and the purpose of it. ... The name(s) or other identification of the person (or class of persons) authorized to request the use or disclosure of PHI.More items...
What are the authorization requirements for use and disclosure of protected health information?
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the ...
What should be included in a authorization for release of information?
The core elements of a valid authorization include:A meaningful description of the information to be disclosed.The name of the individual or the name of the person authorized to make the requested disclosure.The name or other identification of the recipient of the information.More items...
What must be on the authorization form to release PHI?
A signature and date that the authorization is signed by an individual or an individual's representative. If a representative is signing the form, the relationship with the patient must be detailed along with a description of the representative's authority to act on behalf of the patient.
What are the 8 requirements of a valid authorization to release information?
Valid HIPAA Authorizations: A ChecklistNo Compound Authorizations. The authorization may not be combined with any other document such as a consent for treatment. ... Core Elements. ... Required Statements. ... Marketing or Sale of PHI. ... Completed in Full. ... Written in Plain Language. ... Give the Patient a Copy. ... Retain the Authorization.
What is the difference between use and disclosure of health information?
In general, the use of PHI means communicating that information within the covered entity. A disclosure of PHI means communicating that information to a person or entity outside the covered entity, or the communication of PHI from a health care component to a non-health care component of a hybrid entity.
What is included in the authorization for disclosure of PHI?
You may disclose the PHI as long as you receive a request in writing. The written request must contain: the covered entity's name, the patient's name, the date of the event/time of treatment, and the reason for the request.
What is the difference between consent and authorization to use patient specific health information?
Consent refers to an agreement by the patient to allow the health-care provider to use this information to carry out treatment, payment, and health-care operations. Authorization refers to the permission for the health-care provider to make specific disclosures not otherwise authorized by law.
What type of legal document has the authority to release information from the health record of a patient?
A HIPAA authorization form is a document in that allows an appointed person or party to share specific health information with another person or group. Your appointed person can be a doctor, a hospital, or a health care provider, as well as certain other entities such as an attorney.
Find and fill out the correct authorization for use and disclosure of protected health information phi doc 1163a
signNow helps you fill in and sign documents in minutes, error-free. Choose the correct version of the editable PDF form from the list and get started filling it out.
The best way to generate an eSignature for a PDF file in the online mode
Are you looking for a one-size-fits-all solution to eSign authorization for use and disclosure of protected health information phi doc 1163a? signNow combines ease of use, affordability and security in one online tool, all without forcing extra ddd on you. All you need is smooth internet connection and a device to work on.
Find out other Authorization For Use And Disclosure Of Protected Health Information PHI DOC 1163A
If you believe that this page should be taken down, please follow our DMCA take down process here.
What is the confidentiality of alcohol and drug abuse patient records?
3 The rule establishes the following content requirements for authorizations to disclose individually identifiable patient health information generated by alcohol or drug abuse programs:
What is a valid authorization?
In addition to the core elements, the rule states that a valid authorization must include: A statement of the individual’s right to revoke the authorization, in writing, and either: A reference to the revocation right and procedures described in the notice, or.
What is authorization for psychotherapy notes?
An authorization for psychotherapy notes must specifically identify psychotherapy notes when a general authorization or research authorization is executed. This can be indicated by the mark of a check box on the current form, or a separate form can be used.
What is an authorization for marketing purposes?
The authorization must also include a statement about any direct or indirect remuneration the covered entity has received or will receive from a third party. An authorization for marketing purposes can be included on the organization’s compliant HIPAA author ization form or a separate one may be created.
What is the general authorization content?
General Authorization content: The rule states that a valid authorization must be in plain language and contain at least the following core elements: A specific and meaningful description of the information to be used or disclosed.
What is the meaning of "authorization" in medical terminology?
The signature of the patient or legal representative. The date on which the authorization is signed. A statement that the authorization is subject to revocation at any time except to the extent that the program or person who is to make the disclosure has already acted in reliance on it.
What does a covered entity have to state?
The covered entity must state that it may not condition treatment, payment, enrollment, or eligibility for benefits on whether the individual signs the authorization, or. The covered entity must describe the consequences of a refusal to sign an authorization when the covered entity conditions research-related treatment, ...
Legal Requirements
- HIPAA
Section 164.508 of the final privacy rule states that covered entities may not use or disclose protected health information (PHI) without a valid authorization, except as otherwise permitted or required in the privacy rule. General Authorization content: The rule states that a valid authorizati…
Compound Authorizations
- An authorization may be combined with another document to create a Compound Authorization only as described below: 1. Research: An authorization for the use or disclosure of PHI for a research study may be combined with any other type of written permission for the same or another research study, including a consent to participate in the research or another authorizatio…
Marketing Authorizations
- The HITECH Omnibus Rule requires a valid authorization be obtained from an individual before the use or disclosure of PHI for marketing purposes involving financial remuneration. The authorization must also include a statement about any direct or indirect remuneration the covered entity has received or will receive from a third party. An authorization for marketing purposes ca…
Sale of Protected Health Information
- The HITECH Omnibus Rule does not permit a covered entity to directly or indirectly receive remuneration in exchange for PHI of an individual unless covered by a valid authorization. An authorization for this purpose must include a statement that the disclosure will result in remuneration to the covered entity. Note: The way remuneration is used pertaining to the sale o…
Substance Abuse
- The Confidentiality of Alcohol and Drug Abuse Patient Records Rule applies to federally assisted alcohol and drug abuse programs as defined by 42 CFR, part 2, section 2.12.3The rule establishes the following content requirements for authorizations to disclose individually identifiable patient health information generated by alcohol or drug abuse programs: 1. The specific name or gener…
Immunizations
- The HITECH Omnibus Rule made access to immunization records easier for disclosure to schools in states where proof of immunization is required by law prior to admission. Written authorizations are no longer required, but an agreement must still be obtained. The agreement may be oral and must come from a parent/guardian, or other person acting in loco parentis, or di…
Voice Authorizations
- In an environment of continuous technological advancement, the term “HIPAA compliant voice authorization” is occurring more frequently. However, HIPAA does not address voice authorizations. Voice authorizations are based on state law. Unless state law mandates otherwise, acceptance of voice authorizations is up to the individual organization whether or no…
Appendix
- An appendix to this Practice Brief, “Appendix A: Sample Authorization Form” is available online in the AHIMA HIM Body of Knowledge.
Prepared by
- Rose T. Dunn, MBA, RHIA, CPA, CHPS, FACHE Angela Dinh Rose, MHA, RHIA, CHPS, FAHIMA LaVonne Wieland, RHIA, CHP
Notes
- “Standards for Privacy of Individually Identifiable Health Information: Final Rule.” 45 CFR Parts 160 and 164. Federal Register 67, no. 157 (August 14, 2002).
- “Standards for Privacy of Individually Identifiable Health Information: Final Rule.” 45 CFR Parts 160 and 164. Federal Register 67, no. 157 (August 14, 2002).
- “Confidentiality of Alcohol and Drug Abuse Patient Records.” 42 e-CFR part 2. http://www.ecfr…
- “Standards for Privacy of Individually Identifiable Health Information: Final Rule.” 45 CFR Parts 160 and 164. Federal Register 67, no. 157 (August 14, 2002).
- “Standards for Privacy of Individually Identifiable Health Information: Final Rule.” 45 CFR Parts 160 and 164. Federal Register 67, no. 157 (August 14, 2002).
- “Confidentiality of Alcohol and Drug Abuse Patient Records.” 42 e-CFR part 2. http://www.ecfr.gov/cgi-bin/text-idx?c=ecfr&rgn=div5&view=text&node=42:1.0.1.1.2&idno=42#42:1.0.1.1.2.2.1.1
- AHIMA. “Analysis of Modifications to the HIPAA Privacy, Security, Enforcement, and Breach Notification Rules under the Health Information Technology for Economic and Clinical Health Act and the Gen...
Popular Posts:
- 1. who wrote the novel the lincoln lawyer
- 2. how to become a scottish lawyer from overseas
- 3. who was dr. gosnell lawyer
- 4. how does arbitration work against a lawyer
- 5. where is the closeest bankrupcy lawyer in otsego county
- 6. how much does it cost for a power of attorney lawyer in indiana
- 7. if a client wins 2 million, how much does a lawyer make?
- 8. people who enjoy being a lawyer
- 9. when did mamsrtin luther change from being a lawyer to a monk
- 10. what is a liberal lawyer